Sean’s lecture covered the latest evidence related to tendinopathy injuries. In great detail he covered the pathology of tendinopathy, imaging modalities for tendons and the effect load has on tendinopathy injuries.
Tendinopathy was previously and incorrectly referred to as tendinitis. This was incorrect as the “itis” part of “tendinitis” implies that the pathology associated with the injury is inflammation based. However, evidence has shown that this is not an inflammation based injury that can be effectively treated with rest, ice and anti-inflammatory drugs. The injury pathology has been shown to be as a result of tendon cell disruption and is now referred to as tendinopathy or tendinosis. Sean explained that this is a very common injury which can affect inactive individuals and the elite athletic population as well as both older and younger population groups. Furthermore, tendinopathy can be present in the various tendon structures of the body including the patella, achilles, adductor, hamstring, lateral elbow and supraspinatus of the rotator cuff group. Tendinopathy injuries are also more common than what may be reported in the literature, since the standardised definition on tendon injury is “missing training or competition”. This definition doesn’t represent the number of individuals who may have tendinopathy related pain but don’t miss training or competition. Associated risk factors for tendinopathy include age (especially Achilles), gender (more prevalent in males), genetic predisposition and a waist circumference of greater than 83cm.
The major clinical features of tendinopathy as stated by Sean include:
- Focal localised pain
- Pain doesn’t diffuse or refer to other areas
- Pain is load dependant
- Increase in load = increase pain
- Pain is generally worse the day after loading
Normal tendons have four major features:
- Flat elongated tenocytes (tendon cells)
- Parallel collagen fibres
- Small proteoglycans (molecules which attract water into tendon)
- Minimal blood vessels and nerves
These are the opposite in tendons that are abnormal in structure. The abnormal tendon features include:
- Activated and round tenocytes (tendon cells)
- Loss of collagen architecture (no parallel alignment)
- Large proteoglycans (more water into tendon creating tendon thickening)
- Increased presence of blood vessels and nerves in tendon
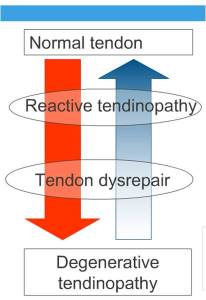
Sean then nicely presented how the evidence shows that there is a sequence of histopatholgical change that occurs within tendons. Stage one is where the tenocytes become increasingly active and rounded. Stage two involves an increase in proteoglycans size. Proteoglycans encourage water to enter the tendon which causes tendon thickening and collagen disruption. Collagen disruption occurs in the final stages of pathological tendon change. However, this can’t occur without changes in tenocytes and proteoglycans. Sean then spoke of the continuum of tendon pathology severity and how tendons can drift between within this continuum (see figure 1).
The stages within the tendon pathology severity include:
- Reactive tendon: tenocytes are activated and increased with an increase in proteoglycans also. Importantly, the collagen fibres are still in a parallel aligned structure. A normal tendon moves into this reactive phase as a result of excessive overloading. With appropriate load management a reactive tendon can return back to normal.
- Tendon disrepair: in this stage tenocytes are still activated and increased as are the proteoglycans. The increased water in the tendon from the proteoglycans start to disrupt the structure of collagen and the parallel alignment becomes compromised. Tendon disrepair occurs if a reactive tendon continues to be excessively loaded. If the collagen disruption is not overly significant, there is the possibility of returning the tendon back to normal. However, the greater collagen disruption that has occurred means it becomes increasingly more difficult to return back to normal tendon structure.
- Degenerative tendinopathy: this stage is where cell (tenocyte) death occurs, collagen is severely disrupted away from the parallel alignment and blood vessels and nerves begin to infiltrate the tendon. A tendon will enter this degenerative phase if it is excessively loaded in the previous stages. It is extremely difficult to return the tendon to normal structure once in this phase, however with adequate rehabilitation and load management the tendon can be asymptomatic.
Once again, this is a continuum which means tendon pathology status could potentially sit in-between phases. For example, tendon pathology may sit between the reactive tendon phase and the tendon disrepair phase.
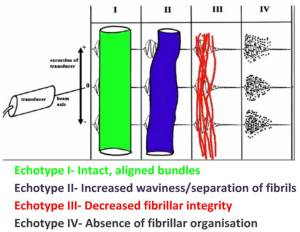
Sean then moved onto discussing the tendon imaging methodologies available and the benefits and limitations associated with them. Traditionally, ultrasound and magnetic resonance imaging (MRI) have been the most commonly used imaging methods. These methods have been reported within the literature as having good to excellent accuracy and sensitivity for detecting clinical tendinopathy. However, limitations associated with ultrasound are that they are highly user dependant. Ultrasound imaging quality can be affected by the quality of the radiographer since image artefacts can be created with a transducer tilt of only ~5°. This can affect diagnosis accuracy. Further limitations of ultrasound and MRI include that these methods are reliant on subjective interpretation for important features such as categorising tendon thickness, grading the severity of tendon pathology and tracking tendon changes over time. A more contemporary method of imaging tendons is the use of ultrasound tissue characterisation (UCT) which was initially developed for use on horses. UCT allows for reliable quantification of tendon structure. A normal ultrasound probe is pulled over the length of the tendon on a motorised track capturing 600 transverse images over a 12cm length. This provides a 3 dimensional image of the tendon. Benefits of UCT include standardisation of transducer tilt angle, frontal/sagital/transverse (3D) images of tendon and the comparison of repeat tendon scans over time. The quantification of tendon structure from UCT scans comes from the level of relative image pixel brightness detected by the imaging device. The output of the UCT scan consists of 4 colours which each represent a different level of tendon structure status/damage (see figure 2).
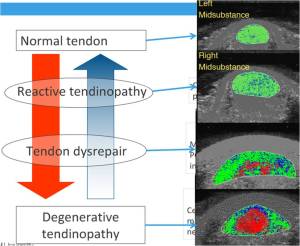
Sean discussed that UTC has been a useful tool for quantifying/staging where on the tendon pathological continuum a particular tendon sits. Figure 3 below shows the relationship between a UTC scan of an Achilles tendon and the tendon pathology continuum discussed earlier.
Since load is a major factor in tendinopathy injury, Sean discussed what load actually is specific to tendons. He discussed load in terms of the intensity of stimulus which is based on the stretch-shortening cycle:
- Low tendon load: tendon stretches slowly without much recoil (e.g. strength training and cycling)
- Medium tendon load: tendon stretches and is required to recoil (e.g. straight line running – not maximal speed and power training)
- High tendon load: tendon is required to undergo significant stretch and recoil at speed (plyometrics, agility and change of direction at high speeds)
When attempting to manage symptomatic tendinopathy, the aim is to maintain some level of tendon loading with low or medium load while minimising the amount of high tendon loading. It is important to keep load in tendons to avoid losing or diminishing tendon capacity which may prove to be problematic when re-loading commences.
I found this lecture by Sean extremely interesting and informative. This was the first time I had heard about the imaging technique of UTC in such detail, and I am really interested in what future knowledge may be gained with this technology. The information Sean presented on the histopathology of tendons was also great.
Profile: Sean Docking
Sean Docking, is physiotherapist and is in the final stages of his PhD studies in the Department of Physiotherapy at Monash University. His PhD research involves the use of Ultrasound Tissue Characterisation (UTC), a new and novel technique that allows measurement of subtle changes in tendon structure that are not detectable using conventional imaging techniques. He has also worked at Carlton football club (AFL).